News
Fax: 931-375-0300
TOA Columbia
Monday-Friday 8:00am-5:00pm
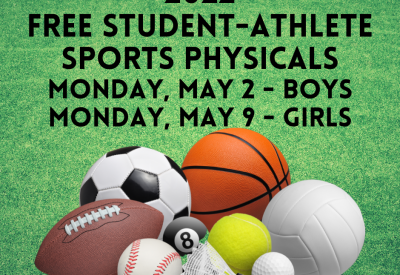
OrthoQuick
Monday-Friday 8:00am-4:30pm Saturday 9:00am-1:00pm
© Copyright 2024. All rights reserved. Privacy Policy. Terms & Conditions.
Design and Development by Muletown Digital